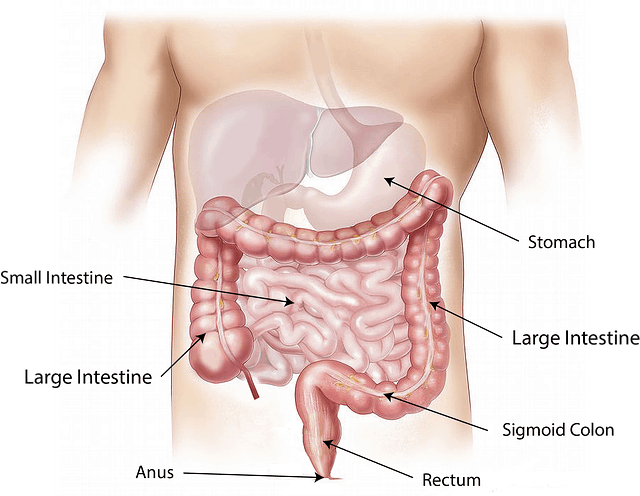
An inguinal hernia occurs when tissue, such as part of the intestine, protrudes through a weak spot in the abdominal muscles. The resulting bulge can be painful, especially when you cough, bend over or lift a heavy object. Some inguinal hernias have no apparent cause. Others might occur as a result of increased pressure within the abdomen, a pre-existing weak spot in the abdominal wall. Strenuous activity, pregnancy, chronic coughing or sneezing. A combination of increased pressure within the abdomen and pre-existing weak spot in the abdominal wall.
In many people, the abdominal wall weakness that leads to an inguinal hernia occurs at birth when the abdominal lining (peritoneum) doesn’t close properly. Other inguinal hernias develop later in life when muscles weaken or deteriorate due to aging, strenuous physical activity or coughing that accompanies smoking. Weakness can also occur in the abdominal wall later in life, especially after an injury or abdominal surgery. In men, the weak spot usually occurs in the inguinal canal, where the spermatic cord enters the scrotum. In women, the inguinal canal carries a ligament that helps hold the uterus in place and hernias sometimes occur where connective tissue from the uterus attaches to tissue surrounding the pubic bone.
Inguinal hernia signs and symptoms include a bulge in the area on either side of your pubic bone, which becomes more obvious when you’re upright, especially if you cough or strain. A burning or aching sensation at the bulge. Pain or discomfort in your groin, especially when bending over, coughing or lifting. A heavy or dragging sensation in your groin weakness or pressure in your groin. Occasionally, pain and swelling around the testicles when the protruding intestine descends into the scrotum. Risk factors that contribute to developing an inguinal hernia include, being male, older or white. A positive family history increases your risk of developing inguinal hernia. Chronic coughing especially in smokers, chronic constipation, pregnancy, premature birth and low birth weight also increases your risk of developing inguinal hernia. Previous inguinal hernia or hernia repair has also been implicated as risk factors.
Complications associated with inguinal hernias include pressure on surrounding tissue which can result in pain and discomfort. Incarcerated hernia which leads to severe pain, nausea, vomiting and the inability to have bowel movement or pass gas. Strangulation can occur causing a cut off in blood flow to part of your intestine and death of affected bowel tissue. A strangulated hernia is life-threatening and requires immediate surgery. You can’t prevent the congenital defect that makes your susceptible to an inguinal hernia. You can, however, reduce strain on your abdominal muscles and tissues, by maintaining a healthy weight, consuming high fiber foods. Lift heavy objects carefully or avoid heavy lifting and stop smoking.
Physical exam is usually all that’s needed to diagnose an inguinal hernia. Your doctor will check for a bulge in the groin area. Because standing and coughing can make a hernia more prominent, you’ll likely be asked to stand and cough or strain. If the diagnosis isn’t readily apparent, your doctor might order and imaging test, such as an abdominal ultrasound, CT scan or MRI. You should be able to gently push the hernia back into the abdomen when you’re lying down. If not, applying an ice pack to the area may reduce the swelling enough so that the hernia slides in easily. Lying with your pelvis higher than your head also may help.
If your hernia is small and isn’t bothering you, your doctor might recommend watchful waiting. In children, the doctor might try applying manual pressure to reduce the bulge before considering surgery. Enlarging or painful hernias usually require surgery to relieve discomfort and prevent serious complications. There are two types of hernia operations, an open hernia repair and laparoscopic repair. Dr. Makemba Shayela Nelson – MBChB – University of Kwazulu-Natal, Durban, South Africa. Nesha Medical Practice.